In the fast-paced world of healthcare, Electronic Health Record (EHR) systems have become indispensable for managing patient health records, streamlining workflows, and enhancing overall healthcare delivery for healthcare organizations.
However, as technology advances, older EHR systems, commonly known as legacy systems, can become outdated and hinder the efficiency and effectiveness of healthcare organizations often leading to clinician burnout.
In this blog post, we will explore the best EHR optimization practices for legacy EHR systems, enabling healthcare providers to enhance existing point-of-care workflows and improve healthcare delivery and healthcare outcomes, enhance patient satisfaction, and achieve seamless system interoperability.
Read below to learn more about our EHR optimization strategies that healthcare leaders are implementing today as part of their overall value-based healthcare strategies.
What is EHR Optimization?
EHR optimization is the process of improving the functionality, efficiency, and usability of electronic health record (EHR) systems. EHRs are digital versions of patients’ medical records that contain their complete health history including diagnoses, medications, lab results, and more.
With the widespread adoption of EHRs in healthcare organizations, there has been a growing need for optimizing these systems to better meet the needs of healthcare providers, patients, and other stakeholders. This involves making changes and improvements to the EHR system to enhance its performance and usability.
What is a Legacy EHR System?
A legacy EHR system, in this case, refers to an often older and sometimes outdated electronic health record system that health care professionals rely on.
Often they are outdated because they don’t meet all the needs and requirements imposed on health care providers as the clinical landscape changes and alternative payment and business models such as value-based care are operationalized.
These systems may have served well in the past, but they pose significant challenges to healthcare providers as technology and the healthcare industry evolve, and patient care requirements change. Legacy systems may lack modern features, impede interoperability with other software, and can become vulnerable to security risks – ultimately leading to physician burnout.
You may be wondering how to improve EHR systems. It is wise to consider an EHR strategy that helps you optimize the system you have.
The Need for Optimizing Legacy EHR Systems
The questions we often hear as an EHR-integration technology provider are just how to improve electronic health records and what you recommend as an overall EHR strategy – especially in light of the shift to value-based healthcare.
Optimizing legacy EHR systems has become crucial for healthcare organizations seeking to provide high-quality patient care while staying competitive in a rapidly evolving industry. Failure to conduct EHR Optimization of your legacy systems can lead to inefficiencies, data inaccuracies, and dissatisfied patients and providers, negatively impacting the overall healthcare experience.
As part of the EHR optimization strategies you implement, healthcare providers can unlock numerous benefits, such as improved patient outcomes, reduced administrative burden, enhanced data security, and increased staff productivity.
Assessing Your Current EHR System
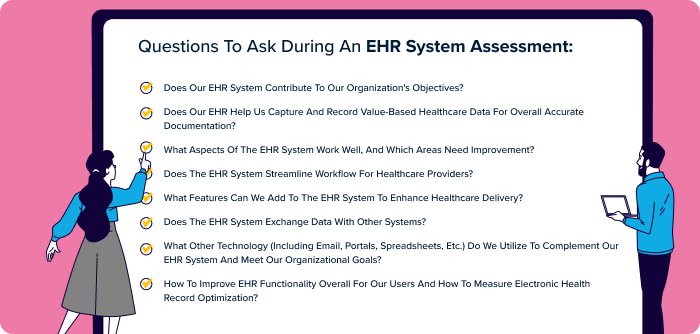
Before embarking on an EHR optimization journey, conducting a comprehensive assessment of your current EHR system is essential. Ask the question – how have EHRs affected the way healthcare is provided? This assessment should encompass the evaluation of system functionality, user feedback, performance metrics, security measures, and interoperability capabilities to achieve robust EHR optimization strategies.
It should also take into account how EHR systems improve the quality of care for patients and analyze if your EHR system has helped your organization achieve improved patient care.
Understanding the strengths and weaknesses of your legacy EHR system will provide valuable insights into what needs improvement and how to strategize for the future – especially when accelerating or transitioning to value-based healthcare.
EHR Optimization Strategies
1. Software Updates and Upgrades
Work with the vendor of the EHR system to identify and apply the latest updates and upgrades. This ensures your system remains compatible with new healthcare standards, maintains data security, and improves overall performance.
2. Interoperability Enhancements
Explore options to integrate your legacy EHR system with other healthcare software applications, such as laboratory systems, billing systems, and patient portals in order to answer the question of how to improve EHR capabilities and work on improving EHR user experience. Interoperability fosters seamless data exchange, reducing redundancy and enhancing collaboration among healthcare providers in addition to contributing to accurate documentation.
3. User Training and Support
Invest in comprehensive training for the staff across the clinical practices in your network to ensure they can make the most of the optimized EHR system. A well-trained workforce can navigate the system more efficiently, improving workflows and enhancing patient care.
4. Data Analytics and Reporting
Leverage data analytics tools within your EHR system to gain valuable insights into patient outcomes, care quality, and operational efficiency. Data-driven decision-making enhances the overall performance of your healthcare organization.
5. Security Upgrades
Strengthen the security measures of your legacy EHR system to protect sensitive patient information from data breaches and cyberattacks. Regular security assessments and updates are essential to maintain compliance with healthcare regulations.
Benefits of EHR Optimization
There are numerous benefits to optimizing electronic health records (EHRs) in healthcare facilities:
Improved efficiency and productivity
One primary benefit of EHR optimization is enhanced efficiency and productivity. Streamlining processes and minimizing manual data entry, optimized EHRs save healthcare professionals time to focus on quality patient care. Quick access to records allows providers to see more patients daily, boosting productivity.
Enhanced data accuracy
EHR optimization improves data accuracy by replacing paper records with electronic systems, reducing human error in data entry. Features like data validation and automated error alerts further enhance data quality.
Improved patient care
Optimized EHRs positively impact patient care. Centralizing all patient information enables healthcare providers to make quicker, informed decisions, enhancing patient outcomes and satisfaction while reducing medical errors.
Better communication and coordination
EHR optimization enhances communication and coordination within healthcare teams. A centralized system provides all members with current patient information, promoting efficient collaboration and benefiting the patient.
Increased data security
EHR optimization boosts data security. Electronic records, protected by encryption and passwords, are more secure than paper-based ones. EHR systems include backup and recovery features, minimizing the risk of data loss.
Cost savings
EHR optimization can lead to cost savings for healthcare organizations. By cutting down on paper records, costs related to printing, storage, and maintenance are reduced. Optimized EHRs streamline processes, lessen administrative burdens, and free up resources for other tasks.
The Impact of Optimized Legacy EHR Systems on Healthcare Delivery
An optimized legacy EHR system can revolutionize healthcare delivery in several ways:
Streamlined Workflows: Improved EHR systems lead to smoother workflows, reducing administrative burdens and allowing healthcare providers to focus more on patient care.
Enhanced Patient Satisfaction: With faster access to accurate patient information, healthcare professionals can provide personalized and efficient care, leading to higher patient satisfaction levels. A goal of all health care leaders.
Improved Clinical Decision-Making: Optimized EHR systems facilitate data-driven decision-making, empowering healthcare providers with real-time insights for more informed clinical decisions. Additionally, it can contribute to fewer medical errors.
Increased Interoperability: Seamless data exchange between different healthcare systems and providers enhances care coordination, leading to better patient outcomes and a streamlined patient journey. This is especially critical in primary health care clinical settings.
Reduced Costs: Efficiency gains, reduced redundancies, and improved resource allocation contribute to cost savings for healthcare organizations.
Conclusion
Optimizing legacy EHR systems is crucial for healthcare organizations looking to provide top-notch patient care, enhance operational efficiency, and stay competitive in a rapidly evolving industry.
By assessing your current EHR system and systems across your network, strategizing for EHR optimization, and leveraging the benefits of modern technology, you can achieve improved healthcare delivery, enhanced patient satisfaction, and seamless interoperability across your network.
And remember, not all EHR upgrades are created equal. A point-of-care technology that can connect data to enhanced workflows directly in provider EHRs is key to ensuring performance at scale.
Want to learn more about successful, technology-enabled payer-provider partnerships?