The healthcare landscape is transforming significantly with the rise of value-based care (VBC) and alternative payment models. In this new environment, the focus shifts from the quantity of services provided to the quality of care delivered and patient outcomes achieved. To thrive under VBC, healthcare organizations need a well-defined strategy.
This blog post offers essential value-based care strategies, helping you navigate this shift and deliver high-value patient care.
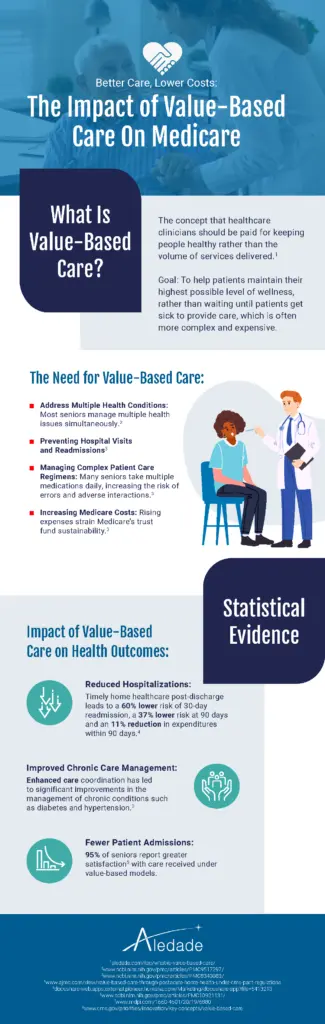
What is Value-based Care?
Value-based care (VBC) is a healthcare payment system where providers (doctors, hospitals, etc.) are financially rewarded for the quality of care they deliver, not just the quantity. Key VBC goals include:
- Better patient health outcomes: Improved disease management, successful preventive care
- Lowered costs: Reducing unnecessary treatments, hospitalizations, etc.
- Enhanced patient experience: Improving patient satisfaction and care journey
Graphic by Aledade
What is a Value-based Care Strategy in Healthcare?
A value-based care strategy is a healthcare organization’s comprehensive plan to thrive within payment models that prioritize the quality of care and patient outcomes over the volume of services provided. This strategy involves a range of actions, including changes in care delivery processes, technology upgrades, and a stronger focus on data-driven decision-making. Let’s break down the key elements:
- Understanding Value-Based Care Contracts: VBC models involve various payment structures, such as shared savings and risk-based contracts. A sound strategy demands a clear understanding of those VBC contracts, the quality metrics that drive payments, and the financial risks and rewards involved.
- Investing in Technology: Robust data analytics platforms, population health management tools, patient engagement technologies, and modern point-of-care and EHR and workflow integration solutions are crucial for success in VBC. These tools empower organizations to track progress, identify high-risk patients, and improve care delivery at scale.
- Prioritizing Patient-Centered Care: VBC success depends on patient engagement, shared decision-making, and a focus on proactive chronic disease management and preventive services. Strategies promote patient self-management support, tailored care plans, and strong communication channels.
- Redesigning Workflows for Care Coordination A value-based care strategy emphasizes seamless transitions of care, reduced redundancy, and proactive follow-up to ensure patients receive timely and appropriate services. This often involves new roles like dedicated care coordinators or navigators.
- Collaborating Beyond the Clinic Walls: Partnering with payers, community organizations, and technology vendors is vital. Collaborations promote aligned goals, shared resources, and innovative approaches for addressing social determinants of health that impact patient outcomes.
A successful value-based care strategy is more than just a one-size-fits-all plan. Healthcare organizations must tailor their strategies based on their unique patient population, capabilities, and the specific VBC contracts they participate in.
6 Value-based Care Strategies
1. Data-Driven Care Management
Robust analytics platforms are the foundation of VBC’s success. These tools aggregate data from various sources (EHRs, claims data, labs, etc.) for:
-
- Population Health Analysis: Identifying trends in disease prevalence, gaps in care, and cost drivers within a specific patient population.
- Risk Stratification: Classifying patients into risk groups, enabling targeted interventions for high-risk and rising-risk patients.
- Quality Metrics Tracking: Continuously monitoring performance against VBC quality measures (e.g., preventive care rates, readmission rates, patient experience scores).
2. Proactive Preventive Care
VBC heavily emphasizes disease prevention and health maintenance. Strategies here include:
-
- Comprehensive Wellness Visits: Regular checkups for screenings, health risk assessments, and patient education.
- Chronic Disease Management: Proactive management programs focusing on conditions like diabetes, hypertension, and heart disease to prevent complications and improve long-term outcomes.
- Immunizations & Screenings: Timely reminders and outreach to ensure patients receive all essential preventive services.
3. Care Coordination
Fragmented care is a significant obstacle in VBC. Strategies for effective coordination include:
-
- Care Transitions Management: Dedicated protocols and follow-up to ensure smooth movement of patients between care settings (e.g., hospital to home).
- Cross-Provider Communication: Streamlined communication channels (both digital and traditional) to prevent information silos and coordinate care plans.
- Care Teams: Multidisciplinary teams (physicians, nurses, care coordinators) that collaborate to manage the complete care journey of complex patients.
4. Patient Engagement and Education
Empowering patients is central to VBC. Key strategies include:
-
- Shared Decision-Making: Involving patients in choices about their care path, fostering buy-in and adherence to treatment plans.
- Patient Portals and Apps: Providing access to medical records, test results, and health education resources.
- Self-Management Support: Offering tools and programs for chronic disease management, lifestyle adjustments, and mental health support.
5. Addressing Social Determinants of Health (SDoH)
While providers can’t directly fix social challenges, here’s what they can do:
-
- SDoH Screening: Identifying factors like food insecurity, transportation issues, etc.
- Community Resource Database: Establishing a network of reliable community organizations to address patients’ non-medical needs.
- Referrals & Follow-up: Connect patients to resources and follow up to ensure needs are met.
6. Partnerships and Aligned Incentives
Success in VBC often hinges on collaboration. Strategies involve:
-
- Payer Partnerships: Aligning goals, sharing data, and exploring innovative risk-sharing models.
- Community Organizations: Partnering to address SDoH, offer educational programs, or provide post-discharge support.
- Technology Vendors: Engaging vendors offering specialized VBC solutions for data analytics, care management, and patient engagement
- Value-based Care Enablers: Organizations that help providers transition to VBC by offering various services. These services can include technological solutions, expert consulting, contract negotiation, and support.

Graphic by Aledade
How Vim Can Help with Value-Based Care Strategies
Vim offers solutions that directly support implementing these value-based care strategies. Our customers work with us to surface their data, insights, and applications for various use cases such as:
- Advanced analytics for risk scoring and population insights
- Risk adjustment and quality performance
- Care coordination tools for patient outreach and care plan management
- Patient engagement technology to facilitate communication and education
- Financial management tools to navigate risk-based VBC contracts
- Partnerships and support resources for transitioning to VBC models
- and more
Conclusion
Transitioning to value-based care demands a comprehensive strategy. By investing in technology, focusing on prevention, prioritizing patient engagement, and fostering collaborations, healthcare organizations can achieve the promise of high-quality healthcare at a sustainable cost.
–
Vim’s point-of-care middleware platform, Vim Connect, surfaces data, insights, and applications that drive performance on value-based and risk-sharing operations where provider care teams are already working—within EHR workflows. Vim’s solutions, including high-value referral selections, quality performance, and risk adjustment, can accelerate the transition to these operations without ever leaving the EHR.
Vim’s solutions are ideal for health plans, developers and product owners, MSOs, VBC Enablers, ACOs, and ACO REACH participants with its provider-friendly and easy-to-deploy software that works across diverse EHRs.



