EHR requirements are the specific features and functionalities that a healthcare practice needs in an electronic health record (EHR) system. These requirements can vary based on the size, type, and specialty of a practice, as well as any regulatory or compliance mandates.
This blog post will provide a guide for healthcare practices to understand and identify their EHR requirements, as well as tips for selecting the right EHR system.
Types of EHR Requirements
There are several types of EHR requirements that healthcare practices should consider when choosing an EHR system:
Functional Requirements
Functional requirements refer to the specific features and capabilities that an EHR system must have in order to perform certain tasks.
These can include clinical documentation, e-prescribing, decision support, billing and coding, and more.
Technical Requirements
Technical requirements are related to the hardware and software specifications needed for the EHR system to function properly.
This includes factors such as compatibility with existing systems, storage capacity, network connectivity, and security protocols.
Regulatory Requirements
Regulatory requirements pertain to any laws or regulations that a healthcare practice must comply with when it comes to managing patient data securely.
For example, practices in the United States must comply with HIPAA regulations to protect patient privacy and security.
Usability Requirements
Usability requirements refer to the overall user experience of the EHR system. This includes factors such as ease of use, intuitiveness, and customization options for different users within the practice.
Why Create a Set of EHR Requirements?
Creating a set of EHR requirements can help healthcare practices in several ways:
Clarify needs and goals
Identifying and understanding the specific requirements for an EHR system can help clarify a practice’s needs and goals. This can also help prioritize which features and capabilities are most important.
Streamline decision making
With a clear set of requirements, practices can more easily compare different EHR systems and make informed decisions about which one best meets their needs.
Ensure regulatory compliance
Having a set of regulatory requirements included in the overall EHR requirements can help ensure that the chosen system is compliant with relevant laws and regulations.
Avoid costly mistakes
By thoroughly considering all types of EHR requirements, practices can avoid investing in a system that doesn’t meet their needs or isn’t compatible with existing infrastructure, potentially saving time and money in the long run.
The cost of EHR implementation and maintenance can also be reduced by avoiding the need to switch to a different system in the future due to missing requirements.
Identifying Your Practice’s EHR Requirements
In order to identify your practice’s specific EHR requirements, it is important to involve key stakeholders in the process. This can include physicians, nurses, front desk staff, and administrative personnel.
Consider conducting a needs assessment survey or meeting with each department individually to gather their input on what they need from an EHR system.
Additionally, consider any regulatory or compliance mandates that your practice must adhere to when determining your requirements.
It may also be helpful to consult with other practices or industry experts to gather insights and learn about best practices.
Once all requirements have been identified, prioritize them based on importance and feasibility. This will help guide the decision-making process when evaluating potential EHR systems.
What Are the Available Capabilities of EHRs?
EHRs aim to improve the overall quality of healthcare by making patient information more accessible and usable, enhancing clinical workflows, and supporting better decision-making.
Each EHR offers a unique range of capabilities that cater to the needs of different healthcare practices. These capabilities can include:
- Storage of patients’ medical history, including diagnoses, medications, treatment plans, immunization dates, allergies, radiology images, and laboratory test results
- Instant access to patient records for authorized users and real-time updates to ensure that all healthcare providers have the latest information
- Efficient data management for large volumes of patient information and detailed reporting for clinical, administrative, and financial purposes
- Patient portals that allow patients to access their health records, schedule appointments, request prescription refills, and communicate with their healthcare providers
- Integration with billing systems for efficient processing of insurance claims and billing, and automation of administrative tasks such as appointment scheduling and management
- Robust security measures to protect patient information, including compliance with regulatory requirements such as HIPAA
- Capability to share and exchange information with other EHR systems, health information exchanges, and external tech solutions
- Tools for analyzing health data across populations to identify trends, manage chronic diseases, and improve public health outcomes
What Are the Meaningful Use Criteria for an EHR?
The 2009 Health Information Technology for Economic and Clinical Health Act (HITECH) is a law created to encourage the “adoption and meaningful use” of EHRs by healthcare practices.
HITECH outlines incentives available to providers and their practices if they meet the criteria that qualify their EHR utilization as meaningful use.
The meaningful use criteria are broken down into three stages.
Stage One
The goal of stage one is to promote the adoption of the EHR. In this stage, covered healthcare providers must meet standard objectives and quality metrics.
When a standard does not apply to a specific provider due to the nature of the care they provide, they can be excused from meeting those criteria.
Stage Two
In stage two, providers must demonstrate advanced workflows and use of their EHR. The criteria expands upon stage one criteria to promote increased information exchange in care coordination.
Stage Three
The goal of stage three is to show improved healthcare outcomes after completing stages one and two.
How to Create a Set of EHR Requirements to Help Evaluate the Technology?
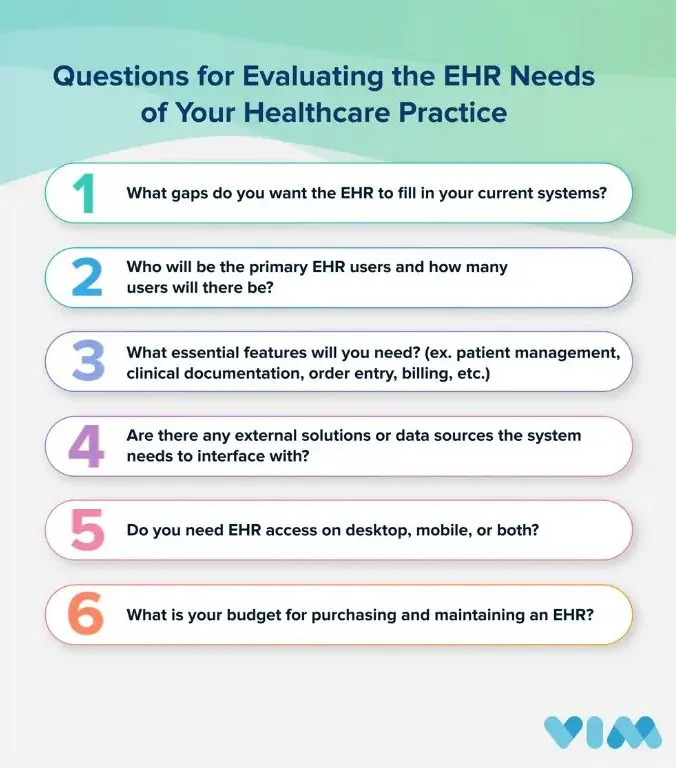
To determine which EHR functionalities will meet your practice’s needs, you must consider its unique characteristics and requirements.
Start by evaluating your needs using the questions below to help you identify your practice’s top priorities:
How to Make the Most of Your EHR Once Implemented
Implementing an EHR can be a challenging process, but it is an important step that can dramatically improve the efficiency of patient care and record-keeping for a medical office.
To maximize its impact, deploying additional tools like Vim can take EHR workflows to the next level.
Vim’s EHR integration technology, Vim Connect, sits on top of the most popular EHRs and enhances provider workflows by delivering patient insights, referral guidance, and more directly at the point of care without third-party EHR dependencies or an expensive and time-consuming integration process.
Conclusion
In summary, EHRs offer a wide array of capabilities that enhance the efficiency, accuracy, and quality of healthcare services.
By identifying the EHR capabilities most critical to a practice’s specific needs, ensuring meaningful use criteria are met, and leveraging tools like Vim for enhanced workflows, providers and healthcare administrators can further optimize the impact of their EHR.
As technology advances, the role of EHRs in healthcare will only grow, making it essential for practices to stay informed and adapt to the ever-evolving landscape of digital health.