Understanding the nuances between value-based care and the traditional fee-for-service model is crucial for both healthcare providers and patients. These two approaches represent fundamentally different philosophies in the delivery and reimbursement of healthcare services. While fee-for-service rewards quantity, value-based care prioritizes quality and patient outcomes.
Below, we delve into the core principles, benefits, and challenges associated with each model to provide a comprehensive overview.
What is Fee-for-Service (FFS)?
Fee-for-service is a traditional payment model in healthcare where providers are reimbursed for every service or procedure rendered to patients. In this model, healthcare costs are based on the quantity of services rather than the quality or outcomes.
While FFS offers flexibility and immediate payment, it has been criticized for incentivizing over-utilization and driving up healthcare costs.
What is Value-Based Care (VBC)?
Value-based care is a contemporary approach that focuses on the quality and outcomes of healthcare services rather than just the number of procedures performed. In a value-based model, providers are incentivized to deliver effective, coordinated care that improves patient outcomes and reduces overall healthcare costs.
This value-based system or model often involves shared risk and shared savings (e.g. risk-sharing agreements) between payers aka private insurers and providers, aligning incentives for better care.
The adoption of value-based care solutions involves establishing partnerships and agreements that share both the risks and savings between healthcare providers and insurers.
This creates a concerted effort towards enhancing patient care and promoting healthcare sustainability by aligning the financial incentives of all parties involved with the health and well-being of patients.
Comparing Value-Based Care and Fee-for-Service
To keep up with these demands, many practices – especially primary care practices – are shifting to the alternative payment model of value-based care that rewards quality over quantity.
Despite the Center for Medicare and Medicaid (CMS) emphasizing alternative payment models and this operational model over the past two decades based on its confidence in its ability to lower healthcare costs and improve the quality of care, the debate over the merits of these two models continue today among healthcare professionals, policymakers, and patients alike.
According to the National Conference of State Legislatures, “In the last decade, the CMS Innovation Center has developed and implemented more than 50 value-based care models across seven categories of initiatives that have been rolled out in all 50 states, Washington, D.C., and Puerto Rico.
Between 2020 and 2022, more than 300,000 providers and plans and more than 41 million individuals with public and private health insurance participated in CMS Innovation Center initiatives.”
Advantages of Fee-for-Service
- Flexibility: Fee-for-service allows providers more freedom to choose treatment plans and procedures based on individual patient needs.
- Immediate/retrospective payment: Providers receive reimbursement for each service rendered, ensuring a steady cash flow.
- Patient choice: Patients have access to a wide range of services and providers, giving them more control over their healthcare decisions.
Disadvantages of Fee-for-Service
- Incentivizes overutilization: The FFS model can lead to unnecessary tests, procedures, and treatments driven by financial incentives rather than what is best for the patient.
- Fragmented care: FFS does not emphasize care coordination, potentially resulting in disjointed or duplicated services.
- Cost escalation: With no focus on outcomes or cost containment, FFS can contribute to rising healthcare costs. According to CMS.gov, “U.S. health care spending grew 2.7 percent in 2021, reaching $4.3 trillion or $12,914 per person. As a share of the nation’s Gross Domestic Product, health spending accounted for 18.3 percent.”
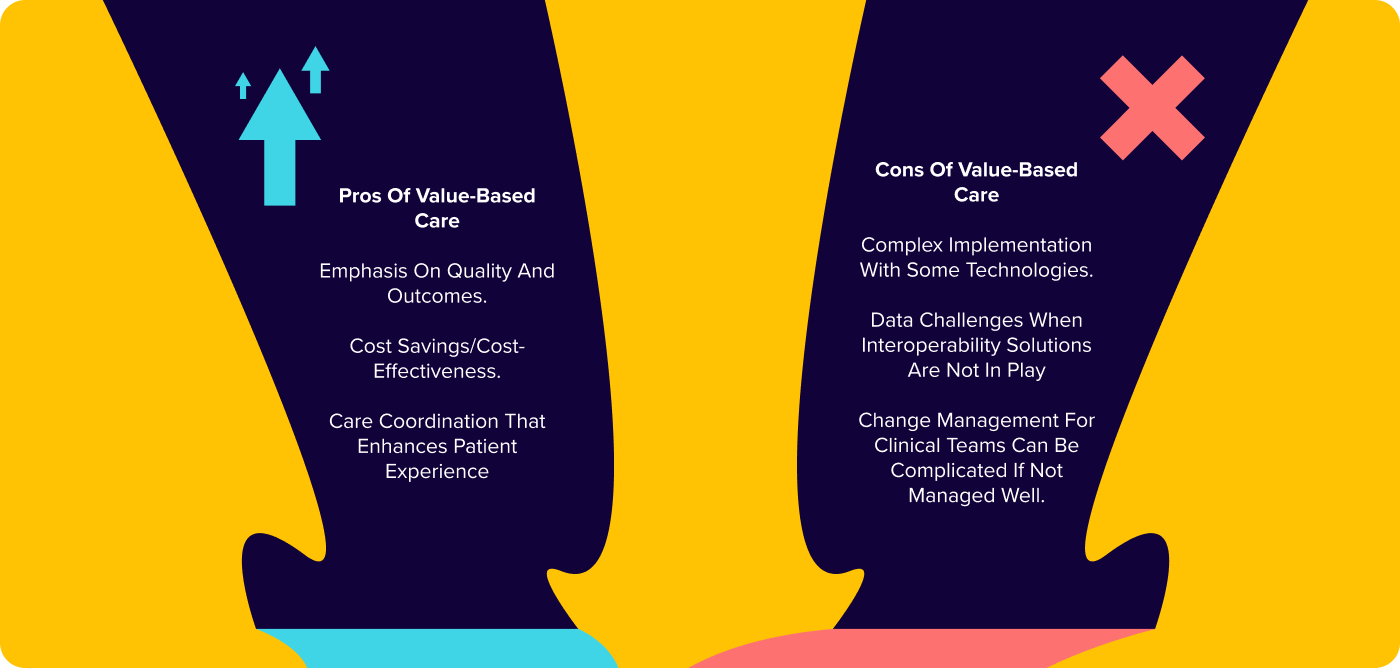
Advantages of Value-Based Care
The pros and cons of value-based care have been debated and analyzed by healthcare professionals, policymakers, and patients alike. Among the advantages of this approach to healthcare are:
- Emphasis on quality and outcomes: A value-based model prioritizes effective, coordinated care that improves patient outcomes and promotes long-term health.
- Cost savings: By focusing on preventive measures and chronic disease management, VBC aims to reduce costly hospitalizations and medical interventions.
- Care coordination: Value-based programs encourage collaboration among healthcare teams to provide comprehensive and patient-centered care, minimizing fragmented services to improve long-term outcomes.
Disadvantages of Value-Based Care
- Complex implementation: Transitioning from FFS to value-based care programs requires significant changes to healthcare systems, including new payment structures and care delivery models. Physician practices often partner with ACOs, value-based care physician enablers, and MSOs to assist with this transition to VBC operations including technology and support services such as contracting.
- Data challenges: Effective VBC implementation relies heavily on accurate and comprehensive data sharing, which can pose challenges in a complex healthcare industry.
Impact of Fee-for-Service and Value-Based Care on Patients
Both FFS and VBC models have specific implications for patient care:
- Fee-for-Service:
- Patients have access to a wide range of services and providers.
- Over-utilization of services may lead to unnecessary procedures or excessive treatments.
- Fragmented care can hinder care coordination, especially for patients with complex medical needs.
- Value-Based Care:
- Emphasizes preventive care and chronic disease management.
- Care coordination improves overall patient experience and outcomes.
- Collaborative approach promotes patient engagement and shared decision-making.
Impact of Fee-for-Service and Value-Based Care on Providers
Both FFS and VBC models have specific implications for healthcare providers:
- Fee-for-Service:
- Provides payment for each service rendered retrospectively.
- Encourages autonomy and flexibility in treatment decisions.
- Incentives may drive some providers to order unnecessary tests or procedures (e.g. quantity of care vs. quality of care).
- Value-Based Care:
- A value-based payment model is based on outcomes and quality, reducing financial incentives for unnecessary interventions.
- Requires care coordination, collaboration, and potentially a significant shift in practice operations and resources.
- Risk-sharing agreements can incentivize providers to deliver high-quality, cost-effective care.
How Does Payment Structure Differ in FFS and VBC?
In a fee-for-service model, providers are reimbursed for each service rendered to patients (i.e. a reimbursement model). This can be on a fee schedule or through negotiated rates with payers. In value-based care, payment structures can vary but often include shared savings, bundled payments, or capitated payments.
These payment models aim to align incentives between payers and providers to deliver high-quality, cost-effective care.
Is Value-Based Care the Future of Healthcare?
The healthcare landscape is gradually shifting towards value-based care as the cost of healthcare skyrockets. As the focus shifts to quality care including patient outcomes, cost containment, and care coordination increases, many healthcare providers and stakeholders are embracing this model.
However, the transition from fee-for-service vs value-based care is complex and requires careful planning, collaboration, and investment in data infrastructure and technology.
Conclusion – What’s Best for You?
The choice between fee-for-service and value-based care ultimately depends on various factors, including individual practice preferences, patient population, and organizational resources. While fee-for-service offers flexibility and immediate payment, value-based care prioritizes quality, outcomes, and cost reduction for overall higher-quality care.
Healthcare organizations must carefully evaluate their goals, patient needs, and available resources to make an informed choice that aligns with their long-term vision.
Looking for technology to put a value-based healthcare strategy into practice?